Fistula in Ano: A Detailed Note
Definition: A fistula in ano, also known as anal fistula, is an abnormal, hollow tract or cavity that connects the anal or rectal lumen with the perianal skin. It is often the result of an infection near the anus causing an abscess, which when drained, forms a tunnel that can become chronic.
Etiology and Pathogenesis: The primary cause of fistula in ano is usually an anorectal abscess, which occurs due to infection of the anal glands located in the intersphincteric plane. These abscesses can be spontaneous or secondary to conditions like Crohn's disease, tuberculosis, trauma, malignancies, radiation therapy, and infections such as HIV or sexually transmitted infections. The persistent infection can lead to the formation of a tract, leading to a fistula.
Symptoms:
- Pain and swelling around the anus
- Discharge of pus or blood
- Irritation of the skin around the anus
- Recurrent abscesses
- Fever and malaise (in cases of systemic infection)
Classification: Fistulae in ano are classified based on their relationship to the anal sphincter muscles. The most widely used classification is the Park's Classification, which divides anal fistulae into four main types:
- Intersphincteric Fistula:
- The tract runs between the internal and external sphincter muscles and opens very close to the anal verge.
- It is the most common type, accounting for about 70% of cases.
- Transsphincteric Fistula:
- The tract crosses the external sphincter and opens on the perianal skin away from the anal verge.
- It is the second most common type, seen in about 25% of cases.
- Suprasphincteric Fistula:
- The tract starts between the internal and external sphincter, goes upwards over the top of the puborectalis muscle, and then descends through the ischiorectal fossa to the perianal skin.
- This type is less common, accounting for about 5% of cases.
- Extrasphincteric Fistula:
- The tract starts at a point high in the rectum or sigmoid colon and travels through the levator ani muscle to the perianal skin.
- It is the least common type and is usually associated with diseases like Crohn’s disease or diverticulitis.
Diagnosis: Diagnosis is typically based on a combination of clinical examination and imaging studies:
- Clinical Examination: Inspection and digital rectal examination to identify the external opening and feel the tract.
- Imaging: MRI is the gold standard for complex fistulae, while endoanal ultrasound can be useful for simpler cases.
- Fistulography: Sometimes used, but less common due to the invasiveness and discomfort.
Treatment: The primary goal of treatment is to eliminate the fistula while preserving continence. Treatment options include:
- Surgical Options:
- Fistulotomy: Cutting open the fistula tract, most effective for low, simple fistulae.
- Seton Placement: A surgical thread is placed through the fistula to help it drain and heal over time.
- Advancement Flap Procedures: Used for complex or high fistulae, involves covering the internal opening with a flap of tissue.
- LIFT Procedure (Ligation of Intersphincteric Fistula Tract): A newer technique involving ligation and excision of the fistula tract in the intersphincteric plane.
- Non-Surgical Options:
- Fibrin Glue: Injection of glue into the fistula tract to close it.
- Bioprosthetic Plug: A plug made of biocompatible material is inserted into the fistula tract.
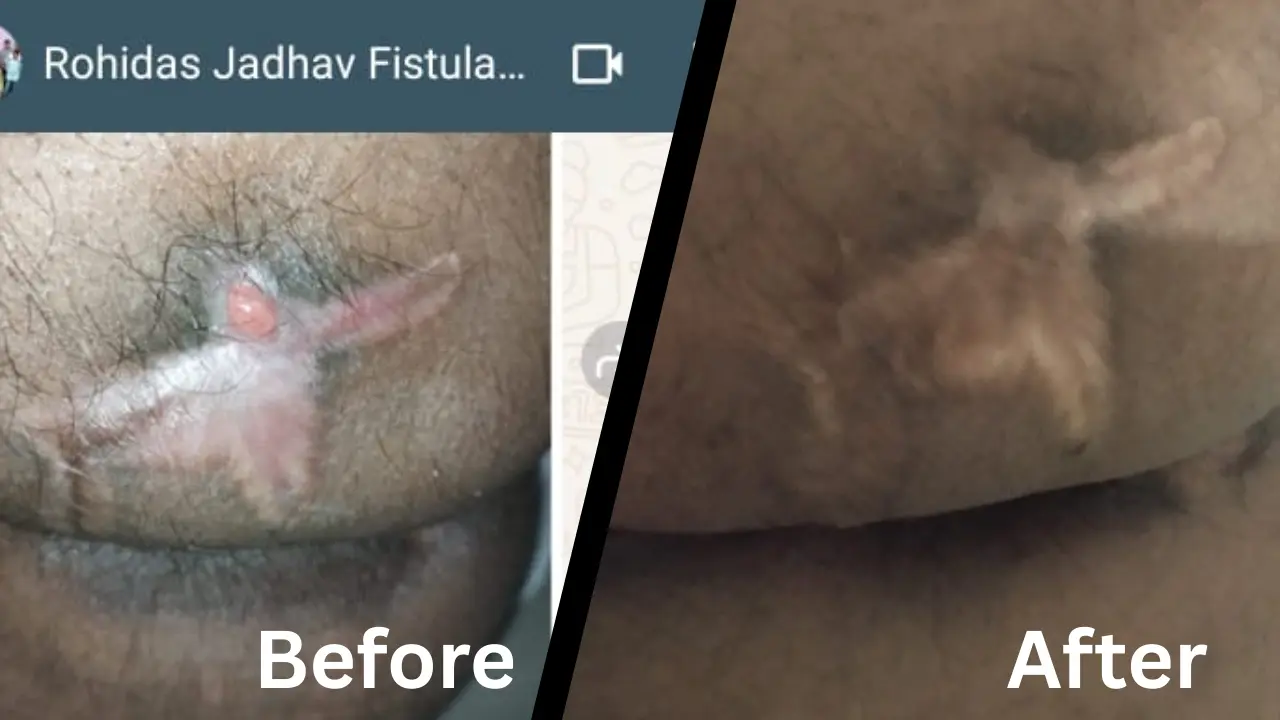
Prognosis: The prognosis varies depending on the complexity of the fistula and the chosen treatment method. Simple fistulae usually have a good outcome with minimal recurrence, while complex fistulae may require multiple procedures and have a higher risk of recurrence and complications.
Conclusion: Fistula in ano is a challenging condition requiring a careful balance between effective treatment and preservation of anal function. Accurate classification and appropriate treatment strategies are essential for successful management and optimal patient outcomes.